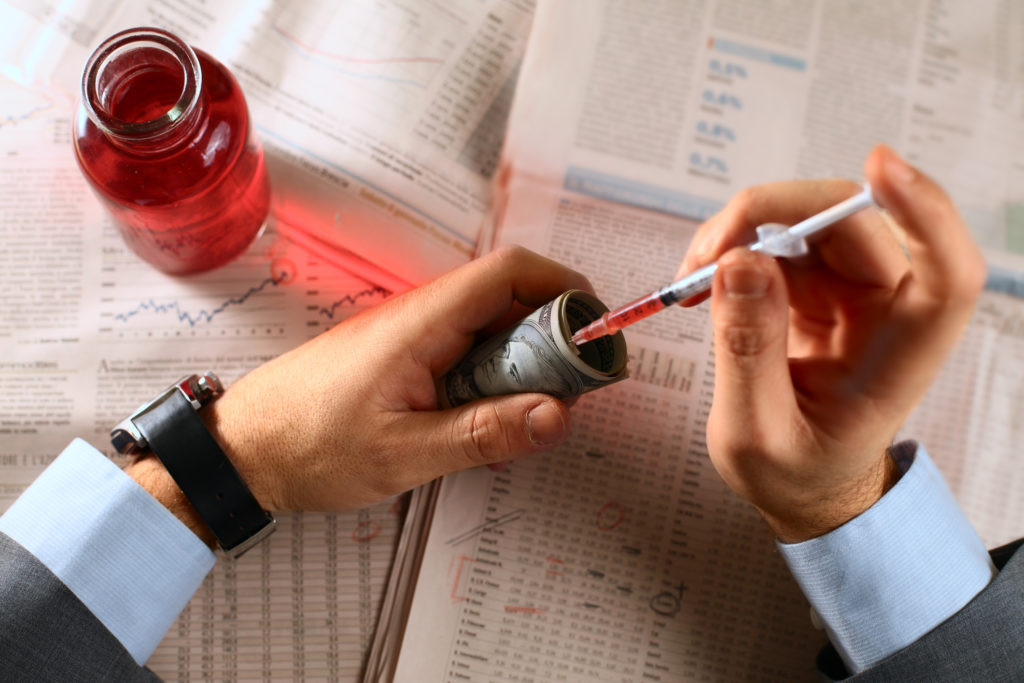
In 2015, spending on prescription drugs grew 9%, faster than any other category of healthcare spending, according to the U.S. Centers for Medicare and Medicaid Services.
The report cited increased use of new medicines, price increases for existing ones, and more spending on generic drugs as the reasons for this growth. Increasingly, though, observers of the healthcare system point to one player – pharmacy benefit managers.
Pharmacy benefit managers are intermediaries, acting as go-betweens for insurance companies, self-insured employers, drug manufacturers and pharmacies. They can handle prescription claims administration for insurers and employers, facilitate mail-order drug delivery, market drugs to pharmacies, and manage formularies (lists of drugs for which health plans will reimburse patients.)
Express Scripts, which provides network-pharmacy claims processing, drug utilization review, and formulary management among other services, is the best-known PBM. CVS Caremark and UnitedHealth Group’s OptumRx are other major players.
A PBM typically has contracts with both insurers and pharmacies. It charges health plans fees for administering their prescription drug claims. It also negotiates the amounts that plans pay for each of the drugs.
At the same time, it creates the formularies that spell out the prices pharmacies receive for each drug on the lists. Commonly, the price the plan pays for a drug is more than the pharmacy receives for it. The PBM collects the difference between the two prices.
It can do this because the health plan does not know what the PBM’s arrangement is with the pharmacy and vice versa. Also, one health plan does not know the details of the PBM’s arrangements with its competitors.
A PBM could charge one plan $200 for a month’s supply of an antidepressant, charge another plan $190 for the same drug, and sell it to a pharmacy for $170. None of the three parties know what the other parties are paying or receiving.
In addition, drug manufacturers, who recognize the influence PBM’s have over the market, offer them rebates off the prices of their products.
In theory, the PBM’s pass these rebates back to the health plans, who use them to moderate premium increases. However, because these arrangements are also confidential, the extent to which these savings are passed back to health plans is unknown. Many observers believe that PBM’s are keeping all or most of the rebates.
To fund the rebates, drug manufacturers may increase their prices. The CEO of drug maker Mylan testified before Congress in 2016 that more than half the $600 price of an anti-allergy drug used in emergencies went to intermediaries.
The PBM’s argue that they help hold down drug prices by promoting the use of generic drugs and by passing on the savings from rebates to health plans and consumers.
They reject the notion that they are somehow taking advantage of health plans and pharmacies, pointing out that they are “sophisticated buyers” of their services. They also argue that revealing the details of their contracts would harm their abilities to compete and keep prices low.
Nevertheless, PBM’s are now attracting scrutiny from Congress, health plans and employers. At least one major insurer has sued its PBM for allegedly failing to negotiate new pricing concessions in good faith. In addition, businesses such as Amazon are considering getting into the PBM business. Walmart is already selling vials of insulin at relatively inexpensive prices.
PBM’s earn billions of dollars in profits each year. With the increased attention those profits have brought, it is uncertain how long that will continue.