2.5 minute read
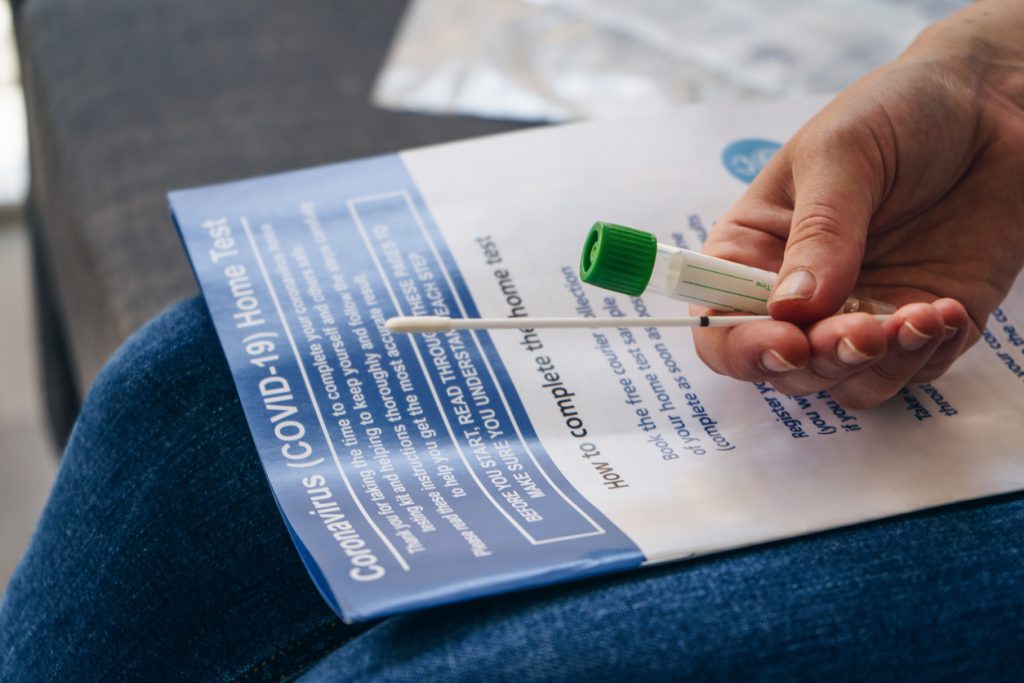
While COVID-19 cases start rising again, more people are once again likely to contract the coronavirus — and that usually involves getting tested. But did you know that you have many options for obtaining a test with no out-of-pocket costs?
Under an executive order issued by President Biden, if you have health insurance you are eligible to receive COVID-19 at-home test kits with no cost-sharing, copay, coinsurance or deductible. Additionally, most health plans are also covering tests performed at hospitals, clinics and pharmacies.
Here’s what you need to know:
Steps for reimbursement
Procedures will vary from insurer to insurer, but the order requires that health insurance carriers reimburse members for up to eight tests a month and no doctor’s order, prior authorization or prescription is required. This applies to any tests purchased on or after Jan. 15, 2022.
Most health plans have preferred pharmacies that they urge their enrollees to go to for their take-home COVID-19 tests. In these instances, the plans will typically cover the cost at the point of sale so that you don’t have to pay out of pocket.
Covering costs upfront eliminates the need for members to submit reimbursement forms.
However, if you go to a non-network pharmacy or drugstore or purchase a kit online, your health insurer is still required to reimburse you for the test up to $12 (or the cost of the test if it’s less than that).
In these cases, you will have to pay for the test upfront and then seek reimbursement from the health insurer.
You can contact your health insurer for information and resources for how you can receive reimbursement. Most insurers have published materials to make it easier for employees to access COVID-19 tests with no cost to them.
Typically, to be reimbursed for at-home test kits, you have to submit a reimbursement form and a receipt that shows proof of purchase, which should include the name of the retailer, including the street address, or, if purchased online, the website address; date of purchase; UPC code for the at-home test kit; and the cost of the test kit.
The order that health plans cover these tests with no out-of-pocket costs for their enrollees will sunset when the federal public health emergency is declared over.
On-site tests
Health plans are also covering the cost of tests that are administered at pharmacies or in hospital settings after either a doctor ordered a test or if the person was exposed to someone who had COVID-19.
Like at-home tests, insurers will cover the costs of these tests regardless of if they are received in-network or from an out-of-network provider or pharmacy.
The types of COVID-19 tests health insurers currently cover are:
- Individual testing with or without symptoms,
- Testing ordered by a health care provider,
- Testing for contact tracing, known or suspected exposure, and
- Testing before or after travel (COVID-19 screening tests for domestic travel are usually covered by most plans, but enrollees should not expect their plan to cover any testing they do abroad).
After the public health emergency ends, however, it’s likely most insurers will stop covering tests obtained out of network.